What Causes Spider Veins?
Spider veins, thin visible veins that sometimes resemble a spider web, are largely a cosmetic concern that doesn’t require medical treatment. However, could your spider veins be a signal of underlying venous disease? What causes spider veins and how can we use these small, superficial veins to diagnose, treat, or even prevent more serious venous health concerns? In this article, we will explore the causes of spider veins and how they can help warn you and Dr. Sergio Verduzco about potential underlying venous disease.
What Causes Spider Veins, And How Are They Linked To Varicose Veins?
Both spider veins and varicose veins are caused by a backup of blood related to venous insufficiency. Venous insufficiency occurs when valves in the veins become damaged or weak, causing blood to pool in leg veins instead of traveling back up to the heart.
Spider veins are also caused by issues unrelated to underlying venous insufficiency, including hormones, sun exposure, and even minor injuries. However, due to their connection with venous insufficiency that can cause bulging, painful varicose veins, it’s recommended that you see a vein specialist for a full evaluation to determine if your spider veins are related to hidden varicose veins in the legs; this will allow your doctors to help you treat venous insufficiency before it becomes a more aggressive problem.
Treatment
Sclerotherapy is a minimally invasive procedure that treats varicose veins and spider veins. It involves injecting chemicals, known as sclerosing agents, into damaged veins.
In addition to diminishing the appearance of varicose or spider veins, sclerotherapy can also reduce pain or side effects caused by damaged veins.
Varicose veins can cause itching, pain, cramping, and discoloration.Spider veins are smaller and less severe than varicose veins. Varicose veins are more common in women than in men, although anyone can get them.
An estimated 20 percent of adults will be affected by varicose veins at some point in their lives. More than 324,000 sclerotherapy procedures were done in the United States in 2017.
Areas that sclerotherapy can treat
The most common areas for varicose veins to develop are on your legs and feet.
The affected veins may be raised, discolored, or swollen, and some are deeper under the skin and can cause discomfort. Spider veins are smaller in size, closer to the surface of the skin, and can appear red, purple, or blue.
More rarely, sclerotherapy may be used to treat hemorrhoids. Sclerotherapy for the treatment of hemorrhoids is typically used when the hemorrhoids are smaller and external. It can also be used when the hemorrhoids bleed or when you can’t risk a surgical procedure such as a hemorrhoidectomy due to other health concerns.
Depending on the size of the damaged veins, sclerotherapy can be used to treat varicose and spider veins in the following areas:
- thighs
- calves
- ankles
- feet
- face (frequently the sides of the nose)
- anus
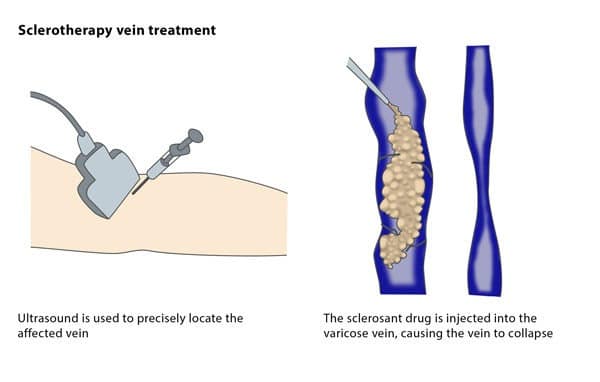
How sclerotherapy works
Depending on the severity of the condition, sclerotherapy treatment for venous problems can take anywhere from 15 minutes to an hour. If you’re getting treatment on your legs, Dr. Sergio Verduzco may have you lie on your back with your legs elevated.
Depending on how far below your skin the damaged vein is, your doctor may use an ultrasound as part of the procedure.
The procedure begins with Dr. Sergio Verduzco cleaning the skin around the targeted veins. With a fine needle, your doctor will inject the damaged vein with a sclerosing agent. Sclerosing agents typically used in sclerotherapy include:
- polidocanol
- sodium tetradecyl sulfate
- hypertonic saline solutions
The liquid or foam solution causes the walls of the injected vein to seal shut, so blood is redirected to unaffected veins. Over time, your body absorbs the damaged vein, making it less visible and uncomfortable.
Based on the size of the treated vein or veins, you may need up to four treatments.